Life and Leisure
Pressure points
(China Daily)
Updated: 2010-09-15 07:53
 |
Large Medium Small |
|
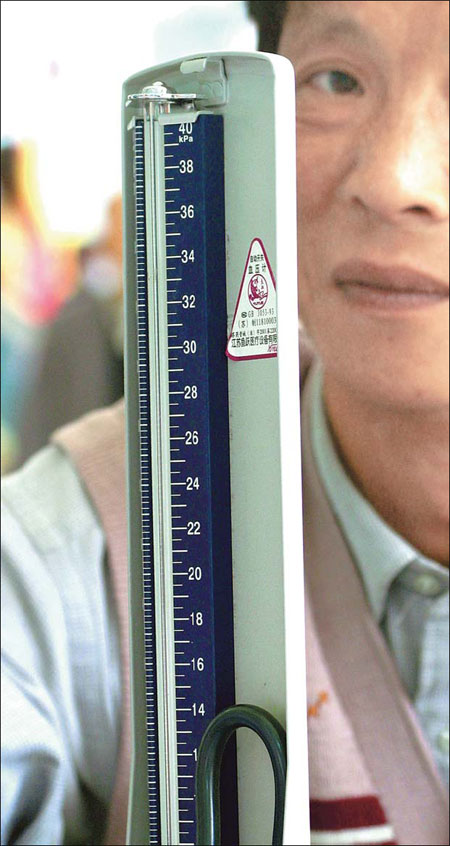
High blood pressure is a leading cause of heart attacks, strokes and kidney failure. Duo Duo / Asia News Photo |
Doctors hope there will soon be an easier way to determine the right drug combination to treat hypertension, which at present is often a case of trial and error.
It's hard to predict which pills will best lower which patient's high blood pressure, but researchers are seeking ways to better personalize therapy - perhaps using a blood test. "The idea that one size fits all doesn't make a lot of sense," says Dr Michael Alderman of New York's Albert Einstein College of Medicine, who supports the blood test approach.
Studies have shown that measuring blood levels of a hormone involved in hypertension can help optimize some people's drug combinations. But, they also revealed that taking a drug that's a poor match to that hormone level might not only fail to work, it may trigger a jump in blood pressure.
Blood pressure is a balance of how much fluid is in your arteries and how tight or relaxed those arteries are. Renin, is a hormone secreted by the kidneys, and the amount in a patient's blood helps determine if the hypertension is a problem of fluid volume or constricted arteries, Alderman explains.
In a study of 954 people prescribed a single drug, those with low renin levels responded best to a diuretic. But people with high renin levels responded better to medicines such as ACE inhibitors that target an artery-narrowing substance spurred by the renin, Alderman says.
Nearly 8 percent of patients had their blood pressure jump at least 10 points after starting medication, the study found. Those most at risk were people who had low renin levels, yet were prescribed anti-renin drugs like ACE inhibitors or beta-blockers.
When doctors see that blood pressure jump, "we always assume that it's the patient's fault" - that they skipped pills or ate too much salt, Alderman says. "It may not be."
But with blood testing now easier and more reliable, some experts say it's time for broader studies to settle the debate.
"We must redirect our efforts away from the strategy of treating hypertension as one condition," writes Wake Forest University public health specialist Dr Curt Furberg. He advocated renin-guided therapy in an editorial accompanying the new research in this month's American Journal of Hypertension.
However, don't expect a routine test for renin, any time soon.
Many doctors are skeptical because initial research a few decades ago failed to show a clear benefit, says Dr Ernesto Schiffrin of Canada's McGill University, a hypertension specialist with the American Heart Association.
"The reality is that trial and error is, to some degree, what has to be done, because patients are different and some patients develop adverse effects with one agent and others don't," he says.
High blood pressure is a leading cause of heart attacks, strokes and kidney failure, and it's on the rise as the population becomes older, fatter and more sedentary. Only about half of patients have their hypertension under control, and the vexing hunt for the right medication is one of the contributing factors to this.
Nearly everyone is urged to start with a diuretic, an old, cheap class of drugs that reduces fluid in the body, and then to add medications that work in different ways as needed. Most people wind up on two or more drugs, and too frequently give up the pill popping, not understanding that it's necessary even when they feel good. Also, many doctors are reluctant to prescribe two- or three-drug combinations until they find the right mix.
In a separate study, Dr Stephen Turner of the Mayo Clinic found that the amount of renin that remained in the blood, while taking a first medication, predicted which additional drug was best to add for further help.
To complicate matters even further, there are racial and ethnic variations. Black patients tend to have lower renin levels than whites, and doctors have long known that for a first drug, blacks fare better with a diuretic than a beta-blocker.
A British study tested two-drug combinations, and found blacks fared worse than whites when mixing another popular medication, a calcium channel blocker, with an ACE inhibitor. But the combination worked far better for south Asian patients, for unknown reasons.
Other researchers think starting everybody on two-drug combinations that hit hypertension from two directions is the way to go. A Canadian study last year supported starting with a low-dose combo of a diuretic plus an ACE inhibitor.
Associated Press